Diabetes & Diabetic Foot – An Overview!
Diabetes and Diabetic Foot: An Ayurvedic Perspective
Table of Contents
Diabetes, if unmanaged, can lead to various complications, one of the most severe being diabetic foot. This condition is characterized by poor circulation, nerve damage, and a higher risk of infections, which can escalate to ulcers, gangrene, or even amputation (Smith, 2020). From an Ayurvedic perspective, diabetic foot is linked to systemic imbalances in doshas, particularly Kapha and Vata, and the accumulation of toxins (Ama) in the body, obstructing proper circulation and healing (Sharma & Patel, 2018).
At the Diabetes Reversal Clinic, under the guidance of Dr. Soumya Hullanavar, a leading Ayurvedic endocrinologist, we provide holistic care for diabetes and diabetic foot, focusing on long-term prevention and management.

Diabetes and Diabetic Foot
What is Diabetic Foot?
Diabetic foot results from long-term complications of diabetes, including (Doe, 2019):
- Peripheral Neuropathy: Nerve damage leads to loss of sensation in the feet, making injuries go unnoticed.
- Poor Circulation: High blood sugar levels damage blood vessels, reducing blood flow to the extremities.
- Infections and Ulcers: Wounds heal slowly due to impaired immune function, increasing the risk of severe infections.
Ayurvedic View of Diabetic Foot
In Ayurveda, diabetic foot is closely associated with Madhumeha (diabetes), a condition caused by:
- Kapha Imbalance: Leads to sluggish circulation and tissue stagnation.
- Vata Aggravation: Causes dryness, cracking, and numbness in the feet.
- Ama Accumulation: Toxins block the channels (Srotas), impeding proper blood flow and healing.
Ayurvedic management focuses on restoring doshic balance, detoxifying the body, and enhancing tissue regeneration (Kumar, 2019).
Symptoms of Diabetic Foot
- Numbness or Tingling: Early signs of nerve damage.
- Swelling and Pain: Indicate poor circulation or infection.
- Ulcers or Wounds: Non-healing sores or blisters on the feet.
- Skin Changes: Dryness, cracks, or discoloration in the feet.
- Foul Odor: May indicate infection or tissue decay (Johnson, 2020).
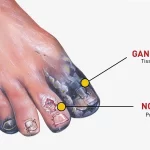
Complications of Diabetic Foot
- Chronic infections.
- Foot deformities due to neuropathy.
- Gangrene and risk of amputation.
- Significant impact on mobility and quality of life (Brown, 2021).
Ayurvedic Approach to Managing Diabetic Foot
At the Diabetes Reversal Clinic, our approach includes detoxification, improving circulation, and promoting natural healing through a combination of therapies, dietary adjustments, and lifestyle modifications (Sharma & Patel, 2018).
1. Detoxification and Cleansing
- Objective: Remove Ama and improve blood flow to the feet.
- Methods:
- Gentle internal cleansing with herbal teas and formulations.
- Panchakarma therapies (optional and customized) to eliminate toxins.
2. Personalized Herbal Medications
- Turmeric: Acts as a natural antiseptic and anti-inflammatory.
- Neem: Helps in wound healing and prevents infections.
- Guggulu: Improves circulation and reduces inflammation (Kumar, 2019).
3. External Ayurvedic Therapies
- Abhyanga (Oil Massage): Medicated oils like Karanja or Mahanarayan Taila are used to improve circulation and nerve health.
- Lepa (Herbal Poultices): Applied to wounds to promote healing and reduce inflammation.
- Swedana (Herbal Steam Therapy): Enhances blood flow and detoxifies tissues.
- Kshara Karma: A specialized Ayurvedic procedure for wound care (Sharma & Patel, 2018).
4. Diet and Nutrition
- Kapha-Pacifying Diet: Include bitter vegetables like bitter gourd and leafy greens.
- Anti-Inflammatory Foods: Use turmeric, ginger, and cinnamon in daily cooking.
- Avoid: Sugary, oily, and processed foods that aggravate Kapha and Ama (Doe, 2019).
5. Yoga and Physical Activity
- Gentle foot exercises to improve blood flow and nerve health.
- Yoga poses like Tadasana (Mountain Pose) and Vrikshasana (Tree Pose) to enhance circulation (Johnson, 2020).
Preventive Measures for Diabetic Foot
- Daily Foot Care
- Wash and dry feet thoroughly, especially between toes.
- Apply medicated oil or cream to prevent dryness and cracks.
- Regular Foot Inspection
- Check for blisters, cuts, or discoloration.
- Use a mirror or ask for assistance to inspect the soles.
- Proper Footwear
- Avoid tight or ill-fitting shoes that can cause blisters.
- Wear soft, breathable socks to prevent skin irritation.
- Control Blood Sugar Levels
- Maintain stable sugar levels to reduce nerve and vessel damage.
- Follow a consistent meal plan and Ayurvedic guidelines (Brown, 2021).
Real Patient Success Stories
One patient shares:
“I had a recurring ulcer on my foot due to diabetes and struggled with slow healing. At the Diabetes Reversal Clinic, Dr. Soumya’s holistic approach, including herbal treatments and dietary changes, helped my wound heal completely. I also learned how to prevent future issues.”
– Patient testimonial (2023)
Why Choose the Diabetes Reversal Clinic?
- Holistic Care: Addressing both the root cause and symptoms of diabetic foot.
- Personalized Plans: Treatments tailored to your constitution (Prakriti) and condition.
- Expert Guidance: Led by Dr. Soumya Hullanavar, a specialist in Ayurvedic endocrinology.
- Sustainable Results: Focus on long-term prevention and management (Hullanavar, 2021).
From the Doctor’s Desk
Dr. Soumya Hullanavar explains:
“Diabetic foot is a serious complication that requires comprehensive care. Ayurveda’s holistic approach not only promotes healing but also strengthens the body’s natural defense mechanisms to prevent future issues.”
– Hullanavar (2021)
Take the First Step Toward Healthy Feet
Managing diabetic foot starts with addressing the root cause and adopting preventive care. Let the Diabetes Reversal Clinic guide you with Ayurvedic expertise and personalized care.
📞 Contact us today: +91 8884722267
🌐 Visit: Diabetes Reversal Clinic
Related-
Know more about Ayurveda Diabetes Reversal Treatments.
GET IN TOUCH
Schedule a Visit
References
Wang Y, Li W, Peng W, Zhou J, Liu Z. Acupuncture for postherpetic neuralgia: Systematic review and meta-analysis. Medicine (Baltimore). 2018 Aug;97(34):e11986. [PMC free article] [PubMed]2.
Çakici N, Fakkel TM, van Neck JW, Verhagen AP, Coert JH. Systematic review of treatments for diabetic peripheral neuropathy. Diabet Med. 2016 Nov;33(11):1466-1476. [PubMed]3.
Dewanjee S, Das S, Das AK, Bhattacharjee N, Dihingia A, Dua TK, Kalita J, Manna P. Molecular mechanism of diabetic neuropathy and its pharmacotherapeutic targets. Eur J Pharmacol. 2018 Aug 15;833:472-523. [PubMed]4.
Alavi A, Sibbald RG, Mayer D, Goodman L, Botros M, Armstrong DG, Woo K, Boeni T, Ayello EA, Kirsner RS. Diabetic foot ulcers: Part I. Pathophysiology and prevention. J Am Acad Dermatol. 2014 Jan;70(1):1.e1-18; quiz 19-20. [PubMed]5.
Vinik AI, Casellini C, Névoret ML. Alternative Quantitative Tools in the Assessment of Diabetic Peripheral and Autonomic Neuropathy. Int Rev Neurobiol. 2016;127:235-85. [PubMed]6.
Elafros MA, Andersen H, Bennett DL, Savelieff MG, Viswanathan V, Callaghan BC, Feldman EL. Towards prevention of diabetic peripheral neuropathy: clinical presentation, pathogenesis, and new treatments. Lancet Neurol. 2022 Oct;21(10):922-936. [PMC free article] [PubMed]7.
Baum P, Toyka KV, Blüher M, Kosacka J, Nowicki M. Inflammatory Mechanisms in the Pathophysiology of Diabetic Peripheral Neuropathy (DN)-New Aspects. Int J Mol Sci. 2021 Oct 07;22(19) [PMC free article] [PubMed]8.
Vinik AI, Casellini C, Parson HK, Colberg SR, Nevoret ML. Cardiac Autonomic Neuropathy in Diabetes: A Predictor of Cardiometabolic Events. Front Neurosci. 2018;12:591. [PMC free article] [PubMed]9.
Sloan G, Shillo P, Selvarajah D, Wu J, Wilkinson ID, Tracey I, Anand P, Tesfaye S. A new look at painful diabetic neuropathy. Diabetes Res Clin Pract. 2018 Oct;144:177-191. [PubMed]10.
Julian T, Glascow N, Syeed R, Zis P. Alcohol-related peripheral neuropathy: a systematic review and meta-analysis. J Neurol. 2019 Dec;266(12):2907-2919. [PMC free article] [PubMed]11.
Gwathmey KG, Grogan J. Nutritional neuropathies. Muscle Nerve. 2020 Jul;62(1):13-29. [PubMed]12.
Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016 Aug 13;388(10045):717-27. [PubMed]13.
Freund PR, Wright T, Margolin EA. Toxic Optic Neuropathy From Quinine Overdose. J Neuroophthalmol. 2020 Jun;40(2):258-261. [PubMed]14.
Guala A, Folgori G, Silvestri M, Barbaglia M, Danesino C. Vitamin B6 Neonatal Toxicity. Case Rep Pediatr. 2022;2022:3171351. [PMC free article] [PubMed]15.
Malet L, Dayot L, Moussy M, de la Gastine B, Goutelle S. [Peripheral neuropathy with hypervitaminosis B6 caused by self-medication]. Rev Med Interne. 2020 Feb;41(2):126-129. [PubMed]16.
Ko JU, Seo H, Lee GJ, Park D. Bilateral sciatic neuropathy with severe rhabdomyolysis following venlafaxine overdose: A case report. Medicine (Baltimore). 2018 Sep;97(37):e12220. [PMC free article] [PubMed]17.
Ly KI, Blakeley JO. The Diagnosis and Management of Neurofibromatosis Type 1. Med Clin North Am. 2019 Nov;103(6):1035-1054. [PubMed]18.
Jani-Acsadi A, Ounpuu S, Pierz K, Acsadi G. Pediatric Charcot-Marie-Tooth disease. Pediatr Clin North Am. 2015 Jun;62(3):767-86. [PubMed]19.
Freeman R. Autonomic Peripheral Neuropathy. Continuum (Minneap Minn). 2020 Feb;26(1):58-71. [PubMed]20.
Kaku M, Berk JL. Neuropathy Associated with Systemic Amyloidosis. Semin Neurol. 2019 Oct;39(5):578-588. [PubMed]21.
Gandhi Mehta RK, Caress JB, Rudnick SR, Bonkovsky HL. Porphyric neuropathy. Muscle Nerve. 2021 Aug;64(2):140-152. [PubMed]22.
Gerischer LM, Scheibe F, Nümann A, Köhnlein M, Stölzel U, Meisel A. Acute porphyrias – A neurological perspective. Brain Behav. 2021 Nov;11(11):e2389. [PMC free article] [PubMed]23.
Abrams RMC, Simpson DM, Navis A, Jette N, Zhou L, Shin SC. Small fiber neuropathy associated with SARS-CoV-2 infection. Muscle Nerve. 2022 Apr;65(4):440-443. [PMC free article] [PubMed]24.
Saif DS, Ibrahem RA, Eltabl MA. Prevalence of peripheral neuropathy and myopathy in patients post-COVID-19 infection. Int J Rheum Dis. 2022 Nov;25(11):1246-1253. [PMC free article] [PubMed]25.
Benstead TJ, Chalk CH, Parks NE. Treatment for cryoglobulinemic and non-cryoglobulinemic peripheral neuropathy associated with hepatitis C virus infection. Cochrane Database Syst Rev. 2014 Dec 20;2014(12):CD010404. [PMC free article] [PubMed]26.
Ferro JM, Oliveira Santos M. Neurology of inflammatory bowel disease. J Neurol Sci. 2021 May 15;424:117426. [PubMed]27.
García-Cabo C, Morís G. Peripheral neuropathy: an underreported neurologic manifestation of inflammatory bowel disease. Eur J Intern Med. 2015 Sep;26(7):468-75. [PubMed]28.
Seeliger T, Prenzler NK, Gingele S, Seeliger B, Körner S, Thiele T, Bönig L, Sühs KW, Witte T, Stangel M, Skripuletz T. Neuro-Sjögren: Peripheral Neuropathy With Limb Weakness in Sjögren’s Syndrome. Front Immunol. 2019;10:1600. [PMC free article] [PubMed]29.
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, Colvin LA, Fallon M. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: A systematic review and meta-analysis. Pain. 2014 Dec;155(12):2461-2470. [PubMed]