Preventing Type 2 Diabetes: Turning Prediabetes Around with Ayurveda
Preventing Type 2 Diabetes: Turning Prediabetes Around with Ayurveda
Introduction
Prediabetes is a warning sign—a stage where blood sugar levels are higher than normal but not yet in the diabetic range. If left unmanaged, it can progress to Type 2 diabetes, increasing the risk of severe health complications like heart disease, kidney failure, and nerve damage. The good news is that prediabetes can be reversed, and Type 2 diabetes can be prevented with timely intervention and lifestyle changes.
Ayurveda, the ancient holistic medical system, offers a natural and sustainable approach to addressing prediabetes by tackling its root causes and restoring balance in the body.
Understanding Prediabetes and Its Risks
What Is Prediabetes?
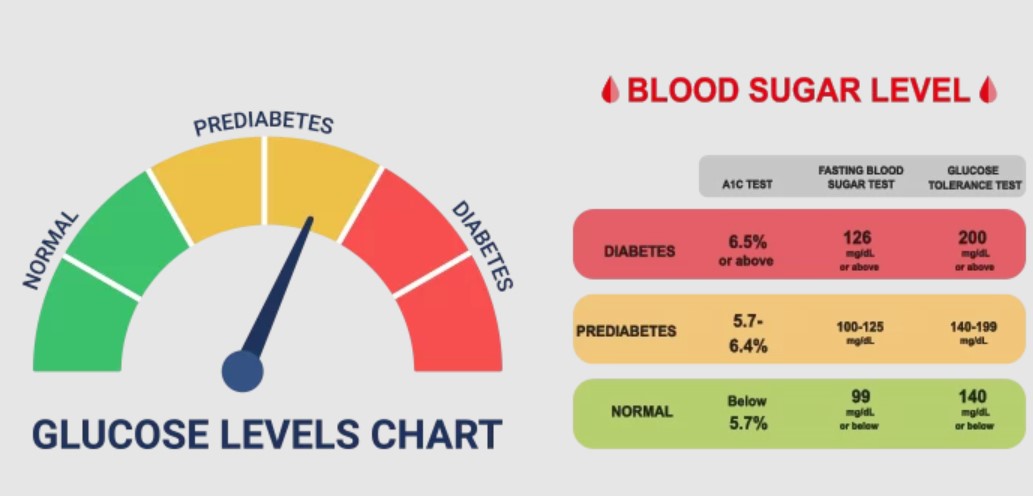
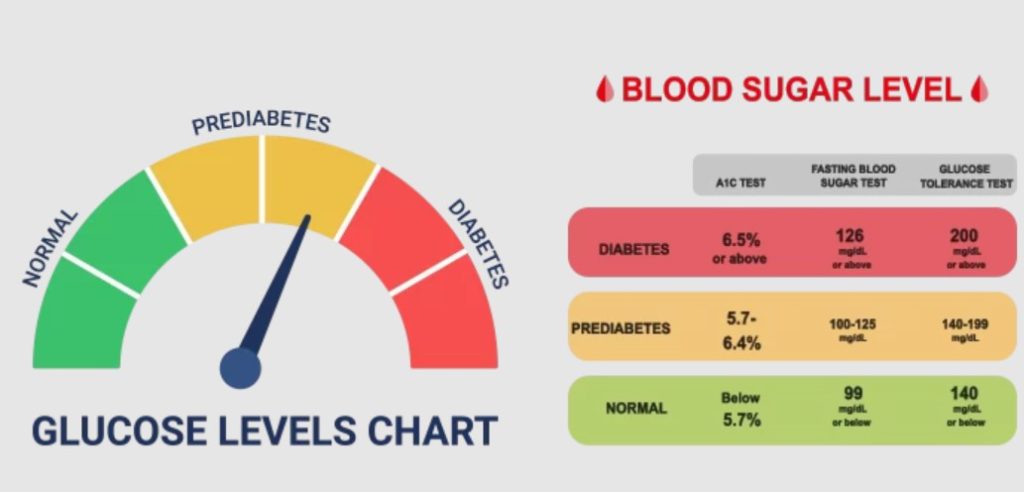
- A condition where fasting blood sugar levels are elevated (100–125 mg/dL) but not high enough to be classified as diabetes.
- It signifies insulin resistance, where the body’s cells do not respond effectively to insulin, causing glucose buildup in the bloodstream.
Risk Factors:
- Sedentary lifestyle
- Poor diet, high in sugar and processed foods
- Obesity or being overweight, especially excess abdominal fat
- Family history of diabetes
- Chronic stress and sleep disturbances
Progression to Type 2 Diabetes:
Without intervention, prediabetes can develop into Type 2 diabetes within 5–10 years.
Ayurvedic Perspective on Prediabetes
In Ayurveda, prediabetes aligns with the early stages of Madhumeha (diabetes), caused by imbalances in the Kapha dosha (sluggishness and buildup) and weakened digestive fire (Agni). Accumulation of toxins (Ama) further disrupts metabolic processes, leading to insulin resistance and elevated blood sugar levels.
The Ayurvedic approach focuses on:
- Eliminating toxins to restore metabolic function.
- Strengthening digestion to improve nutrient absorption and blood sugar regulation.
- Balancing Kapha and other doshas to enhance the body’s natural ability to process glucose.
Turning Prediabetes Around: Ayurvedic Strategies
1. Dietary Adjustments
A personalized diet can significantly improve blood sugar control and reverse prediabetes.
- Low-Glycemic Foods: Emphasize whole grains, fresh vegetables, and legumes.
- Kapha-Pacifying Diet: Focus on light, warm, and easily digestible foods.
- Reduce Sugar and Refined Carbs: Avoid processed foods, sugary beverages, and high-fat snacks.
- Include Digestive Spices: Incorporate turmeric, cumin, ginger, and cinnamon (in moderation) to support metabolism and digestion.
- Regular Meal Timings: Eating at consistent times stabilizes blood sugar levels.
2. Physical Activity
Exercise enhances insulin sensitivity and helps maintain a healthy weight.
- Daily Walks: A brisk 30-minute walk improves glucose metabolism.
- Yoga: Poses like Tadasana (Mountain Pose) and Vrikshasana (Tree Pose) strengthen the core and balance metabolism.
- Strength Training: Light resistance exercises increase muscle mass, which helps regulate blood sugar.
3. Detoxification (Shodhana)
Ayurveda uses gentle detox therapies to eliminate toxins (Ama) and improve metabolic health.
- Herbal Cleanses: Gentle detox drinks or herbal decoctions support liver and kidney function.
- Panchakarma: Therapies like Virechana (purgation) and Basti (enema) are effective for Kapha balance and toxin removal.
4. Stress Management
Stress increases cortisol levels, which can spike blood sugar.
- Meditation and Breathing Exercises: Pranayama techniques like Nadi Shodhana (Alternate Nostril Breathing) calm the mind and reduce stress.
- Mindfulness Practices: Activities like journaling or mindfulness walks help manage emotional triggers.
5. Personalized Herbal Medications
Ayurvedic practitioners at DRC by EliteAyurveda prescribe personalized herbal formulations to:
- Support insulin sensitivity.
- Enhance digestion and nutrient absorption.
- Reduce inflammation and improve circulation.
These medications are tailored to each patient’s constitution (Prakriti) and specific health needs, ensuring optimal results.
How DRC by EliteAyurveda Can Help
At DRC by EliteAyurveda, we specialize in reversing prediabetes and preventing Type 2 diabetes with a holistic, root-cause approach.
Our Program Includes:
- Personalized Care: Tailored dietary plans, lifestyle recommendations, and herbal medications.
- Integrated Therapies: Combining Ayurvedic treatments with lifestyle changes for sustainable results.
- Ongoing Support: Regular follow-ups to monitor progress and adjust the plan as needed.
Case Study: Preventing Type 2 Diabetes with Ayurveda
Patient Profile:
- 38-year-old female diagnosed with prediabetes.
- Symptoms: Fatigue, frequent thirst, and weight gain.
Ayurvedic Intervention:
- Personalized Herbal Medications: Designed to improve insulin sensitivity and digestion.
- Dietary Adjustments: Low-glycemic diet with Kapha-pacifying foods.
- Physical Activity: Daily yoga and a 30-minute walk.
- Detoxification Therapy: A gentle cleanse to eliminate toxins.
Outcome:
- Blood sugar levels normalized within 4 months.
- Increased energy levels and a 10% reduction in weight.
- Improved overall well-being with no progression to diabetes.
Conclusion: Take Action Today
Prediabetes is a reversible condition, and with timely intervention, you can prevent Type 2 diabetes and its complications. Ayurveda’s holistic approach addresses the root causes of prediabetes, empowering individuals to regain control of their health through natural and sustainable methods.
At DRC by EliteAyurveda, we’re here to guide you on your journey toward optimal health.
Take the first step today.
📞 Contact us at +91 8884722267
🌐 Visit our website: diabetesreversal.clinic
